
BRAIN SURGERY
By Chris Dacus 7/15/2018
.
You are probably curious like everyone about the word “brain surgery”.
If those words don't scare you then pinch yourself, congratulations you're not human. Everyone is scared of “Brain Surgery”. It's not for the meek but neither is Parkinson's. it's the last thing you would have done. Just the idea of a brain surgery haunted me for the months leading up to the surgery. This was compounded by my friends, and my family who were equally nervous about my brain surgery.
I had a choice of San Francisco or Boston. I decided to go to Boston for two reasons for brain surgery; one is the great medical community and other is that I have family in Boston where I could stay.
In 2017, I started this journey with my Mom and Fletcher. We went to see my neurologist in Boston, Dr Veronique Van Der Horst who examined me and recommended a neurosurgeon for a Deep brain stimulation, Dr. Ronnie Alterman at Beth Israel Deaconess Medical Center. She said he was excellent. Dr. Alterman is one of those rare doctors who is on top of their game. He is a full professor at Harvard Medical School with 73 published articles on Deep Brain stimulation and Head of Neurosurgery at Beth Israel Deaconess Medical Center. You couldn’t find a better resume for a brain Surgeon. Well actually you can he has only 1/2% of operations go wrong and he's performed over 2,000 deep brain stimulation surgeries. I was confidant that Dr Alterman was the best. If you need DBS surgery by all means go to Dr. Alterman.
So the course was set. I returned to Honolulu to make arrangements to meet the neurosurgeon and his team in early 2018. I had an “on-off” exam at Dr Bruno’s Office then set up the remainder of the tests to be evaluated for DBS which included, a depression exam, cognitive exam, MRI, and a meeting with a social worker and a counseler.
I returned to Boston 5 months later for another set of early morning appointments with Mom and Fletcher. I met a bunch of different team members leading up to Dr Alterman. First we met Dr. Fox, a well known neurologist and DBS prgrammer. Dr Fox is amazingly an electral engineer and a neurologist. That must have been some hard years in college being a dual major for such demanding areas of focus. Needless to say, Dr Fox is smart, very smart. He will be the DBS programmer. I had to complete a MRI of my brain. It was during this visit waiting in the waiting room that I met a woman whose husband had recently have DBS surgery by Dr. Alterman. I asked her what her thoughts were on the procedure. her words were “Dr. Alterman is a miracle worker”. Okay, well that's pretty compelling.
Then there was Patricia Baum, neurological researcher who was a very warm and reasssuring presence and was kind enough to walk us to meetings and make arrangements amidst her real work. Later I would appreciate her even more during the brain surgery. Patricia walked us to Dr. Ronnie Alterman’s office.
Dr. Ronnie Alterman gave me the impression that he was very confident. You could think he was cocky but rather I got a sense that he was a perfectionist. He did everything himself, He sets the bar high for himself .
Many would argue that style is not important, I would argue it is the most important for for me, because it indicates to me a couple things: one is that he is perfectionist, 2. that he's confident and 3 he does everything himself. That is exactly what I was looking for in a brain surgeon.
I always ask doctors one question. “If you were in my shoes, would you do this?” He confidently said he would absolutely do this procedure. He said the surgery could be done with or without anesthesia. He said being awake has greater accuracy. Naturally I asked him if there's any painful part of the procedure. He said that for about 15 minutes when they put this frame on your head. He said they can't put any local anesthesia for the two screws that they had to put in your ear but that these are important screws since they are the alignment of the frame for the rest of the surgery. He made me a little nervous when he said. “all you have to do is last 15 minutes”. He sounded pretty serious.
The surgery was set for June 27th. it was also convenient for me to go Bill Presley's celebration of life which was very important to me. My Ewa Beach family gave me party. it would be an opportunity for me to express my gratitude to the Presley family who gave me the gift of a career of landscape architecture.

The last couple days were particultarly emotional for me. I was honestly nervous about the ability to be the same person after the surgery who entered the surgery. But I kept telling myself I have the best surgeon for this task. That was the argument. It was like a roller coaster. During the pre-operation check and routine CT scan, a nodule in my right lung was discovered. The surgery was delayed until they could figure out what was going on. All I could think of was a big ‘c’ word “cancer”.
A day passed. No news. A couple more days passed. Every day my mother would ask “have they called yet?’ Still no news. Then like an angel, Patricia emailed me “that they would be good news tomorrow”. We would learn that the big day was going to be July 12th.
The night before Cheryl and I decided to have password that we would reserve for after the surgery. Just to make sure I was the same person. My key word was “Pineapple Princess.” Her keyword was “Lub ba dub.”
The morning of the operation, I woke up at 4 in the morning. I had to take a scrub shower with a antiseptic liquid before going to the operation. I finished with my shower at 5 a.m. and the drive to Boston lasted less than an hour. I waited in the waiting room for my name to be called.
After ten minutes, we proceeded to the pre-op rooms. I was called into the pre-op room where preparing for the procedure begins. A nurse came in first and took some vitals. A few minutes later the anesthesialogist, Peter, put in an IV and then he introduced me to Dr. Bose another anesthesiologist. Then one or two nurses came in with the last person to enter was Dr. Alterman. Peter said he was going to begin administering local anesthesia to the locations of the screws. he said it was sting like a bee. I remember it was quite a few locations. also remember that he applied enough that it was dripping down my forehead and my neck.
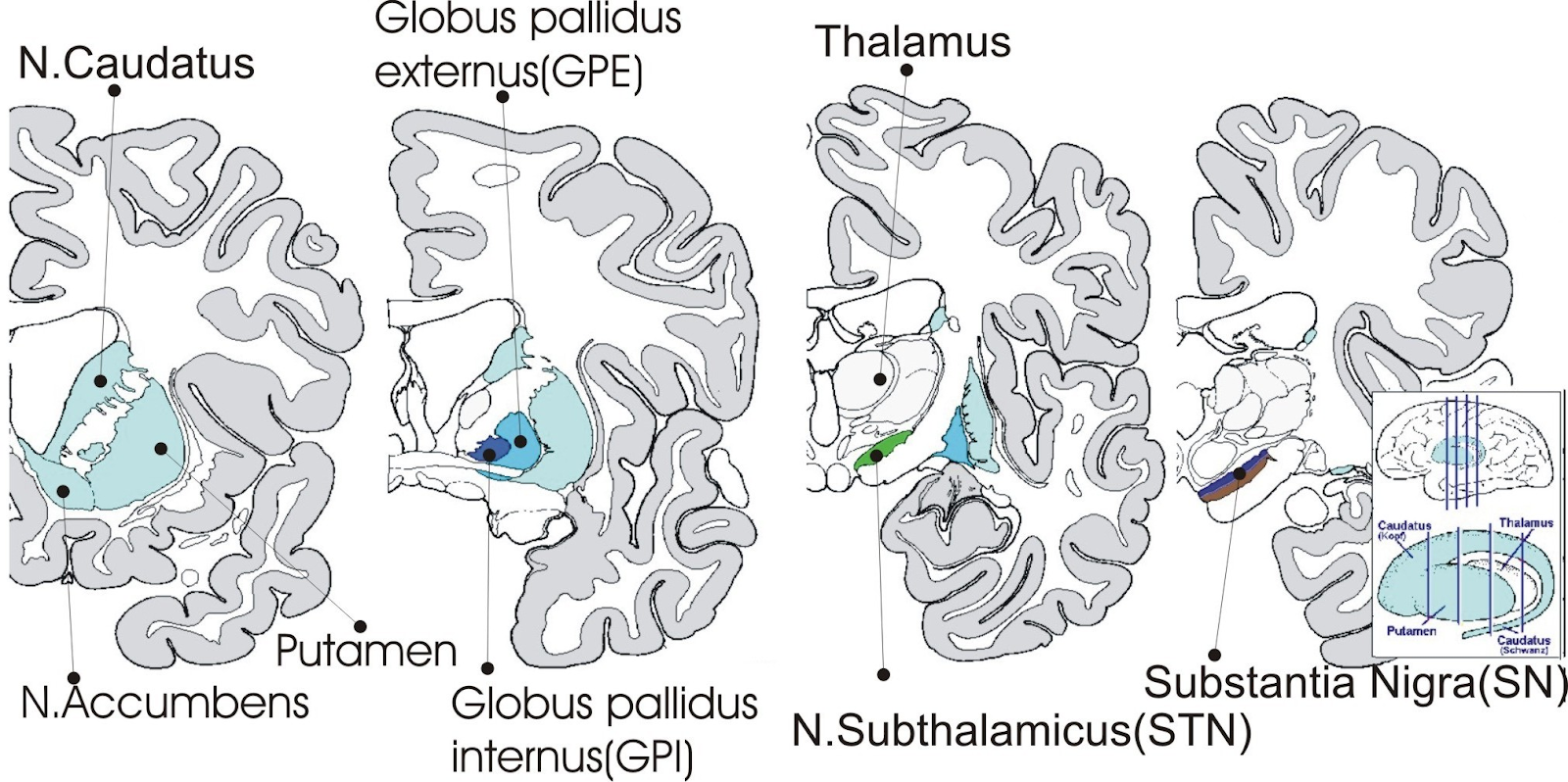
Dr Alterman said good morning. He said he talked about the procedure with Dr. Fox and they came to the consensus that the best placement for me would be the globus pallidus internus. Not the subthalamic nucleus. I responded that i trusted their expertise in making that decision. Fortunately Dr Alterman is trained in both. At this point, the frame was delivered to the room. The frame came gift wrapped in blue paper with a string binding it.
Dr Alterman quickly opened the package and I was looking at a square frame. the frame came in pieces. Dr. Alterman had a pretty intense look as he started assembling the frame with precision.He used a unusual shaped screwdriver. You can tell he's done this hundreds or thousands of times. At about this point, he mentions to me that it would not be shameful to cry or make noises from the installation on the frame. The five people in the room were all looking at me with a penetrating stare.
It was the Moment of Truth. I was either going to succeed and live better or fail and suffer mobility problems. There's only one answer for me -- move forward!

When the doctor walked over and put the frame of my head, I knew right then that it was Game Time. I knew that it was going to painful. I didn't know how painful at that time. He started threading the first ear bar for the right ear and turning the screw until it became painful. Then very painful. I grimaced. My head tilted down. He proceeded without hesitation threading the left ear bar for the left ear. It quickly went from painful to very painful. And I mean very painful. I could have bitten down on something. I felt the pain coursing through my head racing from one side to the other. I was in so much pain from the ear screws, I didn't feel the four corner screws going into my skull. What I did feel was Dr Alterman pushing and tugging the frame to make sure the frame was on well. I felt like Hannabal Lector in “Silence of the Lambs”. He was methodical and didn’t hesitate . Looking back I was thankful that the time was kept to a minimum. The frame was my mask to prevent me form eating other people. As we proceeded to the MRI, I could feel blood dripping down the back of my neck.
In 1949, a Swedish physician, Lars Leksell, introduced the stereotactic frame, a surgical treatment that permits the accurate positioning of probes inside the brain or other parts of the body, based on three-dimensional diagrams.
I was wheeled in for a CT scan in the OR and Dr Alterman determined the alignment for everything to follow. Then Dr. Alterman proceeded to give instructions about tilting the table so he would have easy access to all parts of the frame. At this point I turned to Peter and said “are you going to put me out for this and then bring it back”
Peter said “no”.
I told Peter “That's okay, I want the best outcome no matter what the pain is”.
I talked to the “nurse in the room” and to Peter about their dogs during this time. They both showed me videos on their phones. I asked Dr Alterman if he had a dog and he said no but if he did, the dog would have to be large enough to hug.”
I asked Peter if he could give me something to relax my nerves. The idea of a drill bit punching a hole iin my skull was disconcerting. Peter asked Dr. Alterman if it was ok and he said yes.
‘Dr Alterman was intensely looking at his computer monitor determining his calcuations for the for the DBS. The screen was divided in 4 equal sections show different views. I was correct after all, Dr. Alterman was a perfectionist, confident, and total expert at this procedure. I felt reassured.
Peter applied some local ansthesia to the two burr drill locations on top of my skull for the DBS I felt two quick and sharp cuts on top of my skull. It felt like a papercut.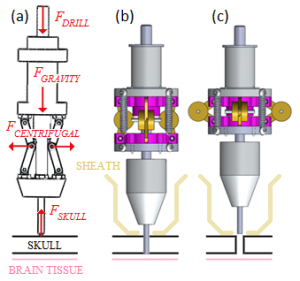
Dr Atlerman asked for suction, a couple times. Once the area was ready, I heard the whirl of an electrical drill. Dr. Alterman quickly made two burr holes. I learned later that a special drill is used, When the drill bit penetrates the skull, it immediately retracts the drill bil preventing damage to the brain. There was no reason to worry after all.
He then screwed two screws which I beleive were used to install a cap on each hole. I didnt feel any pain but i felt the sensation of the screw being screwed in.

After another 10 minutes, Dr Alterman inserted the electrode for the left side. Then he instructed an aid to turn on the electrode. As soon as he said that I felt my body relax. It was an odd sensation after 5+ years of constant rigidity to feel my body relax so suddenly. Wow this could be awesome. I belive what happeneed next was increasing the power to the electrode. Dr. Alterman asked me how I felt. I didn’t feel anything odd and my body was relaxed. After a moment, he said now lets do the right side.
I am not sure but I think he drilled the second burr hole at this point, screwed the plastic cap and proceeded to insert the electrode.
IT occured to me at this point that this is the last real opporuntity for something to go wrong. I waited for what seemed like 5+ minutes for Dr. Alterman to reappear in front of me to ask his asistant to turn on the DBS. I breathed a sigh of relief. Then the DBS was turned on and again my body relaxed. With the operation complete, the frame was taken off the head.
At this point, the doctor had the head end of the bed lowered and he performed one last CT Scan to ensure the electrodes were in correctly. My lower back immediately started to ache. I asked Peter if anything could be done, and he said the doctor is looking for the right location. Be patient” The doctor said “everything is ok, and rolled me back to a flat position.
About 10 minutes went by and they wanted me to complete a second MRI to confirm the placement and cessation of bleeding, and then like an angel, Patricia, a warm and friendly spirit, walked in and said hello and asked me how I was doing. It was so nice to have someone who was the opposite of the brutality of the procedure. Then they rolled me down a second time to the MRI and after the first scan of five minutes, I asked to be let out. I did not want to go back. The operator said I had to do this to complete the DBS and that they would medicate me to a point where I could accomplish this. I woke up in the 3rd visit to the MRI as it was completed. I was wheeled back to recovery and then to a room at the neuro floor and saw my lovely wife. My wife whispered in my ears lubuhdub. I was a little bit confused for a moment and she said lubuhdub again and I remembered my secret password pineapple princess and she smiled from side to side.
Next up: the installation of the new transmitter in my chest.

INTERMISSION: Between the two operations
At this point, I have been in Boston for 5 weeks. I kept myself pretty busy spending my weekdays in Concord writing and photography and weekends in Falmouth/ Woods Hole flying drones, playing ukulele, and watercolor painting. My version of a “still life” drawing…pill bottles.
I spent the next 5 days recovering from the first surgery. The double rows of staples are on each side of my head were painful enough to warrant oxycodone to relieve the pain. I didn’t realize how traumatic the first operation had been--especially the medieval aspect of the head frame.
rested. At least 2-3 times a day, I realized how fortunate the outcomes were. I didn’t take the first surgery lightly - I smiled every day thankful for having completed the brain surgery.
I had some anxiety about the next surgery requiring an MRI in that old machine with the narrow opening. I called the doctor’s office and they confirmed no MRI. Yay:)
SECOND OPERATION: Neurostimulator implantation - July 17, 2018
The first surgery installed two electrodes to the globus pallidus area of my brain. This second surgery was scheduled to remove the staples, attach the wires to go to the chest, replace the staples, tunnel the wires from each side of my head to my upper chest and implant two neurostimulators. I was fully asleep for this entire procedure.
The morning of the operation, it’s deja vu. I woke up at 4am in the morning. I had to take a scrub shower with a antiseptic liquid before going to the operation. I finished with my shower at 5 a.m. and the drive to Boston lasted less than an hour. I waited in the waiting room for my name to be called. I am back for round two with the same nurses in the pre-op room.
She said that I had the reputation from the first surgery as the “friendliest” patient ever. All I really did was talk to each person. A couple of staff shared their dog videos on their phones. The staff were really nice people. Our conversation kept me occupied and helped me to be upbeat during this surgery.
The nurse and physician’s assistant hooked up the IV and the next thing I knew I was in the recovery room. Hmm I was really looking forward to the anaesthesiologists saying count down from 100. Oh well, funny thing is when I awoke I thought that I was lying on the grass in a forest. For about 30 minutes I drifted in and out of consciousness. After the surgery, Dr. Alterman informed my Mom and Fletcher that I was ok and gave them the Medtronic remote control and manuals. About an hour passed and I was totally conscious, eating and drinking as much as possible to get the out of the hospital. About 20 minutes later, they put me in a wheelchair and the nice staff person took me to the outside of the hospital so that we could leave. The pain meds were working well and little did I know that that would soon change. Fletcher picked us up and we drove back to Concord. There was a certain exuberance to be done with the two operations and see the end of the road. When I got home,I facetimed Cheryl, talked and she noted that I had additional breasts than before. That was new to me and was unanticipated. Immediately after the two Medtronic neurostimulators in my chest has caused a slight bump caused by the swelling of the surgery. After a couple days my additional breasts had disappeared.
The pain from the surgery required the use of oxycodone. Unfortunately the second surgery required the removal and replacement of some of the same staples from the first surgery so the healing process had to start from scratch.. The double rows of staples was itchy. After 5-6 days the pain went away and I could wash my head in the shower.
I was totally surprised to hear that Steve Sue was coming to Boston and wanted to sit down and talk story. We met at the “Middle East” restaurant in Cambridge for some appetizers and beer. He presented an amazing hand made lei with notes from my running friends. After all I had been through it was a little emotional. It was just what I needed to pick me up. I am so lucky to be part of such an incredible community in Hawaii. Mahalo nui loa!


The staples were removed 30 July with the sensation of stinging bees. It stung for about 30 minutes. It dawned on me that the staple removal was the end of the pain. Yay!! Now I just had to wait until August 6 for the activation of the neurotransmitters for the first time. For the next week the anticipation was overwhelming. It never left my mind. I felt like an addict awaiting my dose. I watched YouTube videos of DBS patients turning the neurostimulators on and off. It was inspiring.They should show nonstop loops of those YouTube videos in the doctor’s office. I know that I am going to be in heaven when they turn it on. However, I will be a wreck by the appointment time because I won’t have any meds in my body for 10 hours prior to the appointment.
I decided to have a celebration of the neurostimulators activation at Walden Pond Later in the same day. It will probably be pretty emotional on Monday to walk into the water without assistance, going for a swim, without tremors, without dragging my foot. I am sure I will smile from ear to ear.
This is been a long journey - 49,026 miles of flying, over a year of planning, countless bills in our mailbox, more pokes, prodding and needles than I ever imagined, the best doctors bar none and the warm, loving and overwhelming support of friends and family.
I often think of myself as someone who has “Fierce Determination”. Once I set my mind to something I generally always do it no matter whether it's 1 mile or a thousand miles. I do not let voices of doubt get the better of me. My wife would say I'm very stubborn. ( ...it’s true) while it may seem I have no doubts. The truth is I have the same doubts as everyone else. My secret is that I remain positive because I believe my best days are ahead of me, i never give up and I am public about it.
The most important thing I have learned over the years is to be very public about my medical challenges. I know it’s custom in Hawaii to be very private about health situations. I respect that and usually that might be best. We are social animals. We can be stronger knowing others have succeeded. We need each other. The challenges I've faced in the last five to ten years have been the toughest challenges of my life. A couple of people have told me that benefited from my sharing of these trials and tribulations. The support I have received from my friends and family have been the difference between success and failure. I get choked up when I think about it. I have the best friends and family, The most powerful thing has been the love I received from friends and family. It has been the difference in overcoming what seemed like insurmountable challenges to me. Being public has definitely helped me to move forward and has helped at least a couple of people. Being public was a very personal choice and it came with reservations but I feel it was the right choice in this circumstance for me.
THE BIG REVEAL - August 6th
I never really slept last night except for 15 minutes which is unusual for me. Parkinson’s does cause insomnia for me but I usually average 3-5 hours a night. My body is just so rigid in every position I never really sleep. When Fletcher and my mother finally woke up I was dead tired. My instructions for my medical appointment today was no medicine after 9pm the night before. This meant my parkinson's symptoms were in full force. It’s pretty ugly. I can’t walk. I freeze. I shake like a leaf. My body tenses up randomly all over my body. I had to be literally carried by my mother and Fletcher from the front door to the car. I couldn't wait to get my DBS Neurostimulator programming at Beth Israel Deaconess Medical Center. I was so happy to see Dr. Fox. He started programming my neural stimulators and almost immediately stopped my tremors. Since I knew most of the dogs of the medical staff I asked Dr. Fox and he said he had a toy poodle. After an hour, the initial programming was complete. The results are nothing less than exceptional! Minimal rigidity, minimal tremors, improved speech, improved writing, face muscles relaxed, first night of uninterrupted 5 hours of sleep in 3 years, and reduced muscle cramping in my toes. But no improvement in walking and the occasional dystonia which were both expected. I feel 20 years younger than last week. Outstanding results.
It’s very exciting as this will only be improved in 3 weeks at the second programming session.
Whats next for me?
In the simplest terms, take better care of myself in terms of things in my control like diet and exercise. Lastly, work on ways to improve freezing gait. My next big goal is to do the 210 mile John Muir Trail from Yosemite National Park...hopefully in 2019 or 2020.
An update 90 days after surgery 10/12/2018
Every day I count my lucky stars because I feel 20 years younger than before the surgery. I am one lucky guy to have had this amazing surgery. I have reduced my intake of Carbidopa from 1700 mg day to 1000-1200 per day And I’m functioning very well At that lower rate. I continue to enjoy improvements which include greatly reduced rigidity and tremors.
An update 150 days after surgery 1/4/2019
Symptoms remain greatly reduced. Minimal rigidity, minimal tremors, improved speech volume, face muscles relaxed, sleeping consistently 5 hours pre night, and reduced muscle cramping in my toes. I feel good enough that I am talking to a past employer to work one day a week from home. In addition I am devoting my time to advocate for Parkinsons Disease.
Originally Written by Chris Dacus 8/8/2018. Updated 1/4/2019.
Motion off




